The Man who Died of Nothing
Karl’s Eichner’s mysterious plunge from larger than life to end of life in 100 days
This story Is a departure for Trent Hills News. It’s the first story I’ve published written by someone else. I am sharing it because I think it is a powerful love story and medical mystery rolled into one. It’s a reminder of how quickly our lives can change and how limited the knowledge of medical experts can be.
It also has a lot to say about the important role that friends and a caring community and health-care system play in our lives. The writer, Janice Eichner, lives on the water in the hamlet of Trent River.
My husband Karl died in bed without warning on July 9, 2022. At 5 a.m. I felt his body stiffen, he uttered “nightmare” and stopped breathing. Despite my frenzied chest compressions and close to an hour’s ministrations by a team of paramedics and firefighters I was certain before they arrived that he was gone.
His abrupt and shocking departure was the climax of a series of bizarre events that began on April 1 of that year and launched him on a dizzying descent that eluded the most sophisticated diagnostic tests and treatments and stumped a team of experienced physicians. A postmortem revealed nothing to explain his illness or death and the mystery remains unsolved. After a lifetime of carefree, drug-free, glowing good health he woke from his nightmare and died in my arms in less than a minute.
---------------------------------------
Background:
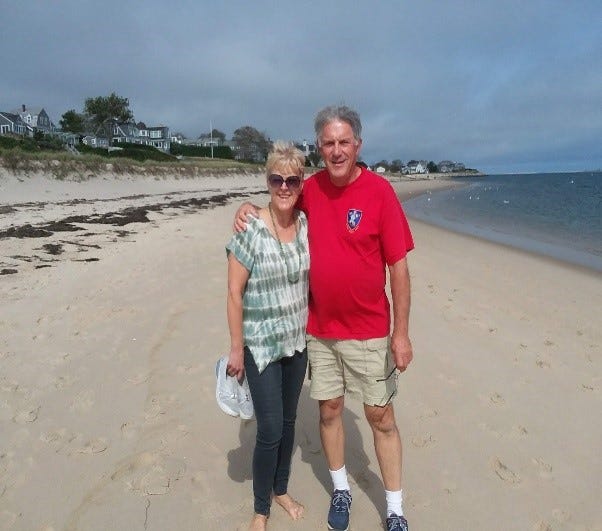
Karl Eichner was a bottomless well of energy – fast walking, fast talking, endlessly cheerful, confident and optimistic about almost everything. When we met at a business conference in Ottawa in 1981, I was literally blown away when he regaled me with amusing stories over dinner, then insisted we take a walk on Parliament Hill in a rain storm so he could point out all the offices where he’d worked as a communications advisor to various cabinet ministers. Even without the tour I would’ve been impressed with this handsome, beaming ball of fire for whom the phrase “force of nature” could’ve been coined. I fell like a ton of bricks. When we discovered we both lived in Toronto it seemed as though it was meant to be.
Karl’s strong personality and Monty Python sense of humour were compelling and sometimes annoying but he quickly became part of my family and circle of friends. My parents weren’t pleased about his brief, failed first marriage but my anglophile nature was drawn to his roots in Northern Ireland and England and his encyclopedic knowledge of history and geography. There wasn’t a flag he couldn’t identify or a capital city he couldn’t name and he knew everything there was to know about geopolitics. He’d lived in and travelled to places as far-flung as Malta, Suriname, Spain and Chile and had a catalogue of stories for every one. Travel become our shared passion and retirement dream.



I discovered early on that Karl was even more of a neat freak than I was, which didn’t seem possible, and from the day he moved into my tiny house in Toronto in 1982 until the day he died I didn’t scrub a toilet, clean an oven or polish a shoe. I simply couldn’t compete.
Karl had arrived in Canada at the age of 17 when his father, a transportation economist, accepted a contract to design airports in the Canadian North. After finishing his last year of high school in Ottawa, Karl returned to the U.K. to serve a three-year commission in the British Army, which paid for his tuition when he returned to Ottawa for a degree in political science and history at Carleton University. By the time we met at ages 29 and 31 we were both established professionals, me in public affairs at RBC and him as vice-president of marketing for Canada News-Wire. We’d both had many relationships (including his short marriage) but each lived alone when we met and were delighted to have found the soul-mate that had eluded both of us. We knew early on we were in it for the long haul.
Although Karl didn’t talk much about his early military experience in Northern Ireland during the Troubles, it was clear that the experience had given him both mental and physical resilience and his consistent good health and good cheer never waned. He was a social drinker but never seemed to feel the effects and despite an aversion to cigarettes and drugs he had a fondness for the occasional cigar as he wandered around doing outdoor chores.
He was fondly considered a bit of a “character” and it was a source of great amusement to our friends that Karl had never in his life had the hiccups or blown his nose. The minor ills he did pick up along the way became another subject of fascination to him. He needed regular polyp checks but relished the colonoscopy prep and refused to be sedated so he could follow it all on the screen. Who needs Netflix when you can watch your colon on TV? His occasional colds, and even Covid, could be sweated out in 24 hours and even when he lost his footing on our crawlspace stairs and sustained a compound crush fracture to his leg on the concrete floor he endured surgeries, casts, pins and plates with uncharacteristic patience and much good humour. It was all another adventure.
While Karl knew he wasn’t indestructible he was confident about his good health and quick to share the wealth when he found out that his Irish blood was particularly useful for cancer patients. The Canadian Red Cross asked him to join its apheresis program in the ‘80s and for decades he supplied white blood cells, ultimately making more than 150 donations.
When we met he was working out at the gym daily, running a 10K most weekends and riding his bike whenever possible. The pace declined as he got older but we were still cycling, snowshoeing and signing up for charity walks until hip pain resulting from his shattered leg slowed him down in the last two years of his life. He compensated with more upper-body tasks like chopping kindling and pulling dandelions. Not a day went by without a “to do” list.
All of this energy and intensity sometimes led to fussiness, impatience and perfectionism that made me wish he could relax more and not over-react to everyday mishaps. He was cool and efficient in a real crisis but small annoyances could frustrate him, particularly if they involved something mechanical that he couldn’t immediately understand. Rather than laugh it off or leave it to someone else, he took the small failures to heart and inwardly punished himself.
Though we had no children in our 37 years of marriage our extended “family” was a group of loved and admired friends all over the Americas and Europe whose friendship was cultivated over a lifetime and with whom connections were never lost. Karl stayed in touch with everyone in his life who meant something to him and was frequently in contact by phone, email and Facebook. He was thrilled when he discovered a British web page called Friends Reunited that put him in contact with an array of childhood schoolmates with whom we later had many happy reunions in the U.K. Our Christmas card list was pages long.
An American friend liked to say that Karl “collected people like some folks collect stamps” and if everyone he’d ever invited to visit us had arrived at the same time, we would have to have leased a multi-storey hotel.
Karl was a natural PR guy and had a long and successful career in public and media relations, ultimately launching his own consultancy and specializing in publicity for trade and consumer shows in Toronto and Ottawa. He was happy to retire to the home we built near on the Trent River but still held onto one client, a large ski resort in Ellicottville, New York where we had a country cottage. Contrary to fears that he’d miss the city vibe, Karl took to rural living like a duck to water and was happiest when he was splitting wood or digging rock gardens.
His lust for life never wavered and although I was younger, I never feared widowhood as I always assumed he’d outlive me. Friends were dumbfounded at the news of his death and many have said, “How could KARL die? He was so full of life”.
I hope someone will be able to answer that question someday.
Seemingly unrelated medical history:
While none of them slowed him down, four diverse medical issues cropped up during Karl’s adult life.
In 2015 he experienced some puffiness in his neck glands and was diagnosed with small lymphocytic lymphoma, a mild and slow-moving cancer that required no treatment other than an annual checkup with an oncologist who ultimately handed the task over to our GP as the condition seemed to be stable. The specialist had said he’d “die with it, not of it” and that turned out to be true. In the months before April 1, 2022, he was bothered by more puffiness in his neck along with some discomfort and hoarseness in his throat. When an ear, nose and throat specialist could find no simple explanation, Karl was referred to another oncologist for assessment. Meanwhile, the symptoms had calmed down and the specialist in Peterborough concluded there was no reason to consider treatment, apart from the usual yearly check-ups.
He had occasional bouts of gout in one big toe, easily corrected with med’s and largely attributed to heredity (we thought) as his father had similar but much more serious episodes. Karl hadn’t had one for more than a year prior to his death.
In 2019 Karl underwent a sleep study after I’d noticed his previously manageable snoring had intensified and the session revealed he had sleep apnea. It was considered moderate, though, as he didn’t experience the arrested breathing incidents typically associated with the condition and when he couldn’t tolerate a CPAP machine there was no further action, except a recommendation that he lose a few pounds.

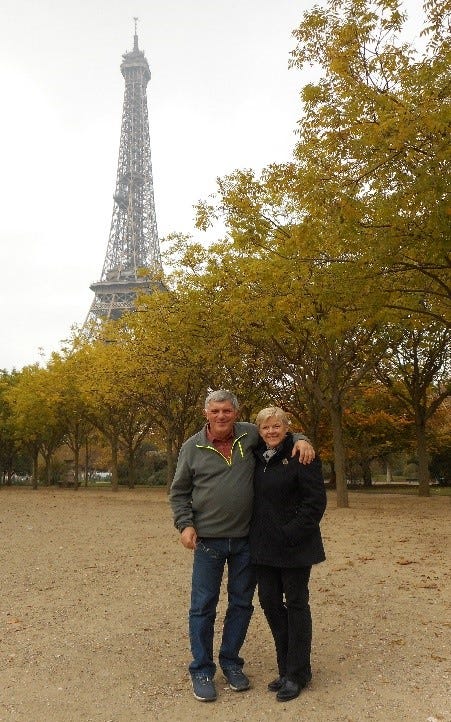

The most mystifying health concern he experienced was in 2018 and it began when he lost consciousness while sitting next to me on a flight to Paris. We were about to land at London Heathrow en route and when I assumed he was sleeping and tried to nudge him awake there was no response. I turned to look at him and his eyes were open but glassy and unmoving and he clearly couldn’t see me. I told a flight attendant I feared he was having a stroke and she ran for a medical bag but by the time she returned he was starting to wake up and seemed confused by all the fuss. He insisted he was fine and by the time we disembarked he was himself again and ate a full breakfast in the airport prior to the next leg of our trip, which went off without a hitch.
We stopped in London on the way home and described the incident to a family friend who’s a neurologist. That doctor’s quite natural assumption was that it was a “vasal vagal” incident, probably involving an electrical circuit in the heart. He recommended a cardiac evaluation when we got back but given Karl’s otherwise excellent health, assumed it was a one-off. If only.
We arrived home from France in a May heat wave and over the next few days Karl lost consciousness with the same glassy-eyed, open-mouthed stare five more times, two of them involving falls that caused minor injuries and triggered calls for an ambulance. As a precaution his driver’s licence was revoked for the rest of the summer and during that time he saw a cardiac specialist, underwent endless tests, including two weeks with a Holter monitor, and had regular ECGs, blood work and even brain screening for seizures. In the end, the diagnosis was nothing more than dehydration, heat stroke and stress. The assumption that it was a heart defect turned out to be a red herring. Karl’s heart was in perfect condition and was even pronounced the “heart of an athlete” when he had a pre-op workup for a hip replacement scheduled for April of 2022 - a long-awaited surgery that never happened.
Oddly enough there was one more passing-out incident in the summer of 2021 during a Face Time call with close friends. I noticed Karl had fallen silent and glanced over to see him staring blankly into space with lips parted as before. I managed to get him from the bar stool he was sitting on into a chair to prevent him from falling and as usual, he recovered consciousness quickly. As he’d been outside in the intense sun, we assumed it was another touch of heat stroke. There was no recurrence then or for the rest of his life.
The diagnosis seemed logical, though, as he’d always been sensitive to heat and was often frustrated by excessive sweating. He had a closet full of coats and gloves that were rarely worn, even in winter, and he’d be in shorts until the snow flew.
I can count on one hand the number of days he was too ill to work and on those rare occasions friends would laugh and declare: “He must be faking it. Karl’s NEVER sick!”

Chronology of illness and death
March 29 to 31, 2022 – Covid-19 had kept us away from our cottage in Ashford Hollow, New York for close to two years and we were keen to be there for a 10-day stay and the first spring clean-up since 2019. We had bought the cozy three-bedroom house in 2007 as a home base from which we could work remotely while our new house was being built in Trent River and it quickly became Karl’s happy place. His city boy persona was the subject of a lot of teasing among our new rural friends and neighbours, but he relished country life and was a keen student of forest management as taught by neighbours who owned the 150 acres of hardwood around us. He could hardly wait to get back there the second the Covid restrictions were lifted.
I worked indoors while Karl raked, cut branches, rearranged our large woodpile and did countless other outdoor chores in mild early spring weather. On March 31, two days after our arrival, he came in at dinnertime complaining of a pain in his right foot and asked me to have a look. The foot was red and inflamed and had what appeared to be a large, flat blister on the top. I declared that he must’ve dropped a piece of wood on it and he applied some antibiotic cream before resting it for the evening and heading to bed.
Friday, April 1 – At 6:45 a.m. Karl hopped out of bed to go to the bathroom and fell to the floor, unable to walk or stand due to the sudden onset of severe spasms in both legs. I tried to help him up but the spasms were too intense. Our neighbours’ friend, a nurse practitioner, was staying next door and came over immediately when I called. She noticed an elevated heart rate and pallor but no other obvious problems apart from the spasms and recommended I call an ambulance immediately.
When we arrived at Bertrand Chaffee hospital in Springville, New York, the emergency room doctor did a quick but thorough check of vital signs and symptoms and declared the problem to be “tick bite paralysis”. Given the season and the growing threat of ticks in our part of the world it seemed reasonable. The discharge instructions noted his condition as cellulitis, which proved to be the more accurate diagnosis, and with a prescription for doxycycline in hand and orders to return if the condition got worse, we headed back to the cottage.
The antibiotics seemed to calm the spasms through the afternoon, but by bedtime they were more severe than ever and rather than go back to the local hospital we decided to pack up and drive home to Trent Hills and our own health-care system the next morning.
Saturday, April 2 – Through the morning the spasms had receded enough that we were able to pack the car and shut down the cottage by mid day. With me at the wheel we crossed the border with no delays and started to hope the worst was past. However, when we stopped for coffee en route and Karl swung his legs out of the car the uncontrollable shakes kicked in again with almost no relief for the rest of the journey. The spasms were in both legs and so relentless and intense that after hours in the passenger seat his lower body was stiff with pain and he was so exhausted he could only stand and walk with assistance. As soon as the car was unloaded, we got back in and headed for Campbellford Memorial Hospital 15 minutes away.
We were lucky it was a fairly quiet night in town and we saw a triage nurse right away. Apart from an unsurprising rise in blood pressure and pulse, all Karl’s vital signs were normal, blood work showed no abnormalities, he had no fever and the rash and swelling on his foot hadn’t gotten worse. The other stroke of luck was that the duty physician was the emergency department chief of staff, an assistant professor of medicine at Queen’s University in Kingston. While all the basic checks were going on he was on the phone to neurology colleagues there and administered some simple brain function tests on the spot, none of which indicated anything abnormal.
Despite the apparent logic of a tick-related diagnosis in tick season the team in Campbellford was skeptical - no evidence of either a tick or a bite and Karl had a reaction that was clearly the opposite of paralysis.
We went home with a prescription for a muscle relaxant in addition to the antibiotic and added a course of prednisone that was originally prescribed to calm down the swelling in his neck prior to his scheduled hip surgery on April 22. The doctor also promised to fast-track Karl for MRIs of his spine and head at our regional hospital in Peterborough.
From Dr. Eshay Elia’s notes on April 2: Over the left foot there is some erythema and swelling – patient says it has gotten a little better since starting doxycycline; the tremor in his legs is best described as a low frequency tonic clonic movement lasting seconds and then settling down; recommend MRI of brain and full spine; advised patient to keep taking doxycycline.



Sunday, April 3 – The spasms eased slightly but persisted, mainly during the night, and on the 4th I wrote this in a note to family and friends:
“We’re cautiously optimistic that Karl’s cocktail of antibiotics, muscle relaxers and prednisone may be starting to calm the leg spasms. He had an uncomfortable evening but a better sleep last night and while his legs were buzzing and jumping early this morning, they settled down around 10 a.m. and have been largely quiet since then. His muscles are badly strained and he’s very tired, presumably from both the drugs and the over-exertion, but if this is the beginning of the healing phase, we’ll be hugely relieved. Too early to say and of course we’ll follow doctors’ orders and forge on with the meds and the MRIs either way but just being able to plan dinner without fearing we’ll be spending the evening at the hospital instead is a bonus!”
Friday, April 8 – The intensity of the spasms in Karl’s legs had eased during the week and while he continued to feel tired and sore, he was cheerful for the first of two MRIs at Peterborough Regional Health Centre. He was one of the first customers in the hospital’s impressive new MRI suite and found the spinal imaging painless, calming and endlessly interesting. We went out for dinner and headed home in much higher spirits, more optimistic than we’d been for a week. Little did we know we were teetering at the tip of the iceberg.
Saturday, April 9 - From Dr. Eshay Elia’s notes: MRI C/T spine reviewed – has some degenerative changes but nothing to suggest a myelopathy; his brain MRI is still pending. I was about to call the patient when I noticed that he was in the Emergency Department.
Sunday, April 10 – Excerpt from my next message to family and friends:
“Karl’s saga is starting to look like an episode of that old TV series House, but without Hugh Laurie around to give us a brilliant diagnosis and instant cure.
“We had hoped for a quiet weekend this time around but Karl had a restless night on Friday and when he got out of bed yesterday he stumbled to the kitchen where I was making coffee and signaled to me that he couldn’t breathe. I helped him to the couch and he managed to get enough air in through his nose that he didn’t lose consciousness while I called for an ambulance but needless to say it was terrifying.
“By some miracle the paramedics made it in five minutes and although Karl was starting to take shallow breaths and ultimately didn’t need oxygen his vital signs were off the chart, and they were convinced he was having a heart attack. I doubted it, given his recent stellar heart test results, but he was back at Emerg in Campbellford and once again no-one could figure out what was going on. He was breathing normally but his oxygen, blood pressure and heart rate were pole-vaulting up and down and to put the icing on the cake a CT scan revealed what looked like two small blood clots in his lung. He finally stabilized when we’d been there about five hours but after they walked him around the room a few times and all his vitals went haywire again they consulted with a cardiologist in Peterborough, put him on blood thinners and admitted him for observation.”
From Dr. Andrew Zohrab’s notes on April 9: Patient states had sensation of throat closing over this morning; throat looks clear; there is no swelling or erythema or palpable nodes in the neck area; blood work including a troponin is essentially unremarkable apart from a D-dimer 5700; CT chest revealed multiple small pulmonary emboli bilaterally; with minimal exertion the patient becomes tachycardic in the 130 range and respirator rate increases to approx. 124; he does maintain 02 saturation.
Monday, April 11 – After Karl had been in the hospital for two days during which his blood pressure descended to normal and his pulse dropped closer to his customary 52 beats per minute he was sent home with no explanation for what had happened beyond a consensus among the docs that the spasms, ambulance runs and crazy leaps in vital signs were most likely related to whatever toxic agent or poison had entered his system by some as-yet-unconfirmed means. A Lyme disease test had ruled out ticks, but spiders and skin-penetrating bacteria were still under consideration and some vials of blood had even been sent to a tropical disease lab in Toronto. Later that day I bought a raised toilet seat with handles to ease pressure on his legs. We’d had a walk-in shower, grab bars and comfort-height toilets installed in our Trent River home when it was built with an eye to our needs 20 years down the road, but had no idea that either of us would need any other assistive devices in the meantime. It was the first of many purchases that added embarrassment to the unease Karl was already feeling.
From Dr. Karishma Bhimji’s notes prior to discharge on April 11: Patient has been ambulated; he did get tachycardic in the 130s however he was completely asymptomatic and his oxygen saturations remained 97-98% on room air; patient feels well; he wants to go home and has an appointment with his oncologist tomorrow; I will put him on a very small dose of beta-blocker bisoprolol since his blood pressure also has been slightly elevated; he will require an echocardiogram as an outpatient; given the small segmental PE and unusual vitals the patient is still tachycardic; he does have some opacities in the left lower lung however he is afebrile and does not have leukocytosis.
Thursday, April 14 – Karl had an echocardiogram at CMH in the morning and a brain MRI at PRHC later in the day. The results of both were completely normal.
Friday, April 22 – We had an hour-long appointment with our local GP, whose experience and judgment we trusted completely, and he was as perplexed as the hospital staff. However, based on everything documented in Karl’s file so far, his best guess was that it wasn’t an insect but a bacterium that had rubbed in through his skin and entered Karl’s blood stream, probably through the foot that erupted in a rash, and caused an infection that ran rampant because his immune system was somewhat compromised by the lymphoma. The fact that a course of doxycycline had worked quickly, at least in the short term, to calm down the severe leg spasms certainly pointed to a bacterial infection.
A physical examination of Karl by our GP revealed some obvious and intense shocks to the system in the form of lost muscle mass. At that point he had dropped at least 10 of his 200 pounds in three weeks. Nonetheless he was determined to get back in shape for his hip surgery, now rescheduled for June. In the meantime, with blood thinners, beta blockers and prednisone now crowding the kitchen counter when a month before he was taking nothing but vitamins, Karl was clearly on the threshold of a strange and unsettling new world. The doctor entered weekly follow-up appointments into his schedule.
April 23 to May 17 – At long last the spasms had subsided and while Karl was still monitored regularly by our GP, he finally seemed to be over the infection. He gradually felt stronger and apart from a slight limp due to his hip he bounced back quickly in typical Karl fashion. He started mowing the lawn and weeding the rock gardens and even waterproofed our large deck. On May 14 Karl drove to the U.S. cottage on his own for a happy few days of R&R. We both felt upbeat and relieved at his progress. I agreed to write an article about his experience for the CMH Foundation newsletter and in addition to praising the staff’s wonderful care and encouraging people to donate, the story was infused with optimism for the future. It was a feeling that soon came to a crashing end.
Wednesday, May 18 – Karl had come back from the U.S. cottage for an appointment with an ear, nose and throat specialist in Peterborough who we hoped would shed light on the persistent swelling in his tongue even though it had calmed down by this point. The doctor couldn’t find anything worrying but requested a CT scan of the neck.
Friday, May 20 – Karl had the CT scan at CMH and the results revealed no issues with any part of his ear, nose and throat system. The doctor’s assessment was “stable, mildly enlarged cervical lymph nodes; no new lymphadenopathy in the neck; all other glands, digestive tract, ventricles, and vascular structures normal.”
Saturday, May 21 – We were busy with a few chores around our Trent River home that morning but started to hunker down at lunchtime in advance of a severe storm forecast for our region on the first day of the Victoria Day weekend. We’d had bad storms and high winds before but the meteorologists warned that it could be a “once in a generation” event. We’re just south of Highway 7, which usually means we get off more easily than areas to the north so were cautious but not particularly worried. When the wind suddenly picked up, the air became heavy, the sky turned black and rain started to fall sideways in huge sheets we resigned ourselves to a proper storm. Shortly after 2 p.m. the power went off and we stared in disbelief as the wind roared in like a train, the river erupted in white caps, tall cedars snapped in two on our lawn and branches piled up all around the yard. Then, with a deafening crash two of our neighbour’s trees succumbed to the blast and hurtled down hard on our roof.
I told Karl we had to get to the crawlspace but he seemed rooted to the spot and for a terrible few moments I realized this could literally be a killer storm. Yet as suddenly as it had come the wind and rain moved off to wreak even more devastation on areas to the east. We stepped outside to assess the damage from what was later confirmed as a rare derecho and found the lawn almost completely covered in debris with an entire 50-foot cedar and the top third of a giant pine perched on the roof, having left our fence, flower beds and eavestroughs in tatters. Our neighbour’s cottage escaped a direct hit but he lost more than 10 trees on his property, one a huge pine that tore down a Hydro line and left a pond-sized hole when it was ripped out by its roots.
We called our builder to come and check the roof and went out to start clearing a path. Karl began to drag huge branches into piles and heave up whatever blocked his way. I urged him to take it easy but he wouldn’t stop. Close friends turned up with a chain saw and the work went on for hours.
Ironically that summer-like day, which started with such optimism, was the beginning of the end.
Sunday, May 22 – We got up early in the morning to carry on with the clean-up, but Karl had wakened with hip and lower back pain after a fitful night. He tried to help but was unsteady on his feet and we assumed he’d further injured his bad hip in the frenzy of hauling logs and branches the previous day. We even wondered about a ruptured disc or sprained sacroiliac as the deterioration and lack of balance had come on suddenly, as had painful spasms in his lower back. By the end of the day, I’d hauled out the walker a friend had loaned to us in advance of Karl’s hip surgery and it became his constant support. The first of nine falls in the house happened a few days later.
Quite naturally, Karl’s relentless good humour was also strained in the aftermath of so many assaults on his system and while we both tried to keep our spirits up, he began inching into a place of anxiety and depression he’d never experienced his entire life. And for the first time since we’d met, I had a cold stab of fear that Karl might be facing a dilemma that couldn’t be fixed.
Friday, May 27 – Excerpt from an email Karl sent to friends and family:
“I saw my GP Brendan Keogh this morning as part of my bacterial infection follow-up. He insists I stay on the beta blockers and blood thinners for a full six months or until told otherwise by my hip replacement surgeon. I mentioned my ongoing insomnia, muscle spasms and the fact I had fallen in the house. He examined me and pointed out that I was extremely tense and several muscle areas were in fact in spasm as we chatted. It is nothing cardiac and my vital signs are good. I am basically stressed out. Big surprise! He noted that over an eight-week period I got an infection that could have killed me, spasms that caused blood clots and stiff muscles, neck lymphomas that thankfully don’t need treatment yet – all these causing delays in my hip surgery. Then voila – a storm that dropped trees on our house and could have killed Janice and me on Saturday. Brendan quipped that I have been living in a perfect storm! So, he told me to slow down and gave me a prescription for stronger muscle relaxers. No martinis for two weeks! The pills should calm me for sleeping at night and reduce the muscle spasms. Only a two-week supply since we want to make sure the hip surgeon is comfortable with my meds. This is wild – two months ago I had never been on prescription meds and now my Norwood pharmacist and I are on first name basis!”
Wednesday, June 1 – Despite Karl’s decline in mobility we decided to drive to Uxbridge for lunch with close friends. He used a cane and leaned on me as we made our way slowly across their large lawn but was clearly uncomfortable, fragile and distracted even while we enjoyed their kind hospitality and upbeat conversation. He was glad we’d made the effort but said on the way home that it had been “too much”. It was so unlike him I had to hold back tears. My friend Linda later admitted that seeing Karl so diminished had been a gut punch to them as well.
Thursday, June 2 – I drove Karl to Campbellford for a professional massage and while his walk into the clinic was painful the treatment was soothing, at least in the short term. His spirits continued to flag as none of the medications seemed to be helping but his customary cheerfulness still prevailed – that is until we were stunned by the unexpected news that a dear friend in Ashford Hollow was in hospital with a heart attack. Terry and his wife Betty were our neighbours up the road and the two “buddies” had formed a strong relationship over more than a decade. Terry had looked after our cottage all through our Covid absence and we were making up for the lost months by spending time together whenever we were there.
Betty kept us up to date as Terry underwent an array of tests and procedures at the hospital in Buffalo but even though there was some early optimism his brave fight to recover ended on June 17. When his passing became inevitable in the last couple of days, we were all given the opportunity to send farewell messages and photos that Terry’s family would share with him. Karl got me up at dawn on the 15th (our wedding anniversary) so I could take a sunrise photo of him standing on the deck toasting Terry with a glass of single-malt whisky, one of the pleasures they had shared. The photo was accompanied by an Irish blessing. When the end came for Terry, it was the beginning of a new and heartbreaking phase for Karl. My brave, pragmatic, stalwart husband, who had only shed tears once in all the years I’d known him, began to dissolve into daily bouts of sobbing. When I wrote the following note to Betty that day, I had no idea we’d both be widows within five weeks:
“Nothing to say except we’re adding our tears to the many that are being shed right now. Karl hasn’t cried for 40 years but they’re flowing freely for his dear pal and confidante Terry. You’re such wonderful friends and we’ll do anything we can to support you in the days ahead. He’ll be with us always and we need to think of him at peace instead of us in pieces.”
Saturday, June 4 – Karl’s nights were increasing restless with physical and emotional pain in a constant tug-of-war and he suggested I start sleeping in the guest room so at least one of us could have a good rest. At the same time, I’d been pondering how we could make getting in and out of bed easier for him and decided to check out options at the Home Health store in Peterborough. I found a sturdy device with a base that strapped securely under the mattress and a metal railing that fitted along the top half of one side of the bed. Since his arms were strong and in good shape he’d be able to grab the bar, pull himself easily into a sitting position and stand with the walker. It turned out to be a brilliant addition but only worked with the guest room bed, not our own IKEA wooden bedframe, so that became Karl’s room for what we hoped would be the short term. He would never sleep in our bed again.
Sunday, June 5 – Karl and I had both contracted Covid-19 in late 2020, months before vaccines became available, and for two years I’d been coping with a chronic long-Covid headache that a neurologist tried for months to treat with powerful migraine drugs. None of them worked so when he referred me to an ENT specialist to explore whether there could be a link with my sinuses, an MRI of my head and neck was scheduled for the first Sunday in June. Karl had been unsteady on his feet but was doing well with the help of the walker and promised that he’d just sit at his desk and work in the office until I got back from the appointment.
I phoned him from the car when I was pulling in and as he swiveled in the chair and grabbed the walker, all three of them – Karl, walker and chair – toppled over and he hit his head on the corner of a wooden wall unit. When I walked in, he was lying immobile in a small pool of his own blood and as I didn’t want to move him, I called for an ambulance. At CMH he was fixed up with two stitches in his head and the doctor’s report confirmed no loss of consciousness, no headache, no vomiting, no vision changes and no neck pain. Karl even joked with the doctor about his first-ever stitches at age 71. He was in good spirits when we got home and blamed himself for a moment of carelessness. Sadly, several more falls in the house made it obvious it wasn’t that simple.
Over the next two weeks the spasms in his back became more intense and were accompanied by jerks in his arm as he tried to put food from a fork or spoon into his mouth. The latter he dismissed as “all in my head”, particularly as depression and a Pandora’s Box of frightening flashbacks to his military service in Northern Ireland had started to set in immediately after Terry’s heart attack. As for mobility, his upper body remained strong and he was able to easily hoist himself out of a chair with his hands on the walker as long as he kept his feet apart. If his feet were together, he was unable to separate them when standing and would start to teeter and fall. When I wasn’t nearby, he’d go down like a felled tree unless there was something he could grab to break the fall. In all, he fell nine times indoors without serious injury before the worst one broke his lucky streak.
Saturday, June 11 – In an effort to make it easier for Karl to get on his feet I’d ordered a lift chair that our local Bennett’s furniture store delivered and set up. It was a comfortable recliner as well and fit nicely into the living room with a good view of the TV. Karl was pleased, although quick to label it his “old man’s chair”.
Thursday, June 16 – Because Karl’s April symptoms had included a sensation of his throat closing, he’d been scheduled for a swallow test at PRHC. We drove in for the appointment and it went without a hitch. The results were perfectly normal.
Saturday, June 18 – Due to Terry’s death the day before it had been a sombre but peaceful day at home in lovely summer weather. Karl felt like a breath of air on the deck around 6 p.m. so made his way out there with the walker to one of the glider chairs, where he communed with nature while I started some dinner prep. I joined him a few minutes later, at which point he wanted to get up and try his luck with some crutches, which he hoped would be an option for him in tight spaces. He’d never had a problem hoisting himself up to the walker and I was standing behind the chair for stability but he teetered as he stood, missed the walker handles and went sideways with a crash onto the deck, falling hard onto his right arm and breaking three bones in his wrist in the process. I rushed to break his fall but couldn’t stop the momentum. The ambulance arrived in about 10 minutes and we were back to Emerg at CMH, where luckily our hero Dr. Elia was on duty. A technician took Karl for an X-ray and the doctor reset the fracture and applied the cast himself but needless to say we were scared and upset, wondering how we could possibly manage back home when Karl needed two strong hands for the walker.
Dr. Elia solved the immediate problem by ordering that he be admitted and confined to bed until a physiotherapist could do an assessment on Monday with a view to finally nailing down what was really going on. He also ordered another MRI since he was alarmed by the deterioration in Karl’s mobility and suspected further injury since the storm.
Sunday, June 19 – From my morning note to family and friends:
“Poor Karl was already verging on depression given recent events and the trauma of Terry’s death less than 48 hours ago so the next few days won’t be easy, particularly as sleep is difficult with the heavy cast. He’d been counting on an orthopedic pre-op appointment scheduled for Wednesday to finally get the hip replacement process back on track but clearly that will have to be postponed. Because of Covid protocols I can’t visit him today but will drop off a bag of essentials that will be taken to his room. The medical services were mercifully quick for a Saturday night in town but it took ages for the admission and preparation of the bed so he was in Emerg until 2 a.m. and I got home about 2:15.
“Karl called at 7:30 a.m. to say he’d managed some fitful sleep but they’re not letting him out of bed except to sit up on the side and presumably get to the bathroom at some point so I’m hoping he’ll be able to nap most of the time away. It’s hard to look on the bright side but we’ve made a list of positives – he’s left-handed so at least his dominant arm is fine, the nurses are kind and cheerful, he’s in a safe place and getting the forced rest he needs so badly and we should be on the brink of some answers this week. My guess is that he may be transferred to PRHC for further tests but whatever happens we’ll just have to cope. I’m aching for him and tired after a short night but otherwise fine and will do my best to cheer him up on the phone.”
Later that day Karl went to PRHC and back by ambulance for the spinal MRI ordered by Dr. Elia.
Monday, June 20 – I took Karl’s iPad and some fresh clothing to the hospital in the morning and was there while the physiotherapy team took him for a monitored walk and some mobility exercises in the hallway. It was tiring but promising and the therapist was happy with the fact that his legs were in good shape, as was his range of motion.
But more important and informative was the floor doctor’s visit with the results of Sunday’s MRI. In addition to the hip deterioration we knew about all too well, it turned out that Karl had spinal stenosis and may even have sustained a herniated disc the day we ran out to clean up after the storm. He was given a referral to a neurosurgeon in Kingston, which was ultimately scheduled for mid September, and due to the wrist fracture his hip surgery was also postponed to the Fall. Despite huge disappointment at yet another delay of his new hip, Karl was relieved to hear that his spinal stenosis was common and probably unrelated to the mobility problem. And however far off it seemed, the promise of a September solution to the mystery gave both of us a much-needed shot of hope.
Sadly, even that didn’t prevent his now-daily downward spiral as the afternoon wore on. Later, I recapped my evening visit for my friend Linda in an email:
“He was pretty spacey when I arrived and as despondent as I’ve ever seen him. He’s in so many different kinds of discomfort they’re trying an array of remedies and I think the one with codeine must’ve knocked him for a loop. He was fretful and fragile and didn’t know what to do with himself. I helped him shave and brush his teeth, which made him feel better, but the best part of the evening was when a kind male nurse came in for a chat and volunteered to organize a shower for Karl courtesy of an equally kind young PSW. They brought in a special shower chair and loaded him up just as I was leaving and he called after I got home to say that he felt 100 per cent better and that Alecia had done a beautiful job washing him. He’s wiped out and was dozing off but the nurse had tucked him up in bed and I’m hoping he’ll get a better sleep tonight.
“Fingers crossed he’ll be in better shape in the morning. I’ll be showing up at 10 to help him into street clothes – shorts, t-shirt and sandals – and we’ll leave in the transfer vehicle about 11:30. We don’t know what the orthopedic surgeon will have to say but at least we’re moving forward.”
Tuesday, June 21 - Karl had had a nearly sleepless night due to the heavy cast on his arm, steadily getting tighter with swelling underneath, and the regular appearance of nurses at all hours to check on him and the elderly gentleman with whom he shared the room. He’d managed a fitful nap before I arrived at 10 a.m. but was pale, drawn and desperate for a wash despite the previous evening’s shower. Personal hygiene was always a priority for Karl and a minimum of one daily shower plus a close shave with a manual razor was his routine. After a lifetime of energy and self-sufficiency, sudden loss of control over his mobility was a special kind of torture.
Later, many friends told me that his emails to them at that time were full of guilt and worry about the toll everything might be taking on me. “Poor Janice already has to do everything around the house and now this! I’m totally useless.”
Nevertheless, we managed to stay cheerful for each other while riding to PRHC and back for the appointment with an orthopedic surgeon who would assess the damage and determine what, if any, surgery was needed. After removal of the cast and a new round of X-rays the doctor’s reaction was “He should’ve been here sooner” due to the complexity of the break. Surgery was scheduled for two days later.
Wednesday, June 22 – Karl had slept better after an exhausting day and some relief from a slightly lighter plaster cast applied by the orthopedic specialist, but his spirits were sinking fast. He lost interest in eating and I could almost watch him shrinking as more pounds rolled off. The previous two nights I’d brought along glasses and a small shot of whisky so we could share a wee dram as visiting hours waned but this time he was too despondent even for that. The only consolation was that earlier in the day a nurse had come in with a wash kit containing an ingenious cap infused with shampoo that I could use to give his head a cleansing massage. We also managed a pretty thorough sponge bath but despite a few smiles as I wielded the washcloth, I could tell he was on the verge of panic at the spectre of long-term dependency.
Karl wasn’t a churchgoer but knew that my minister, who he’d met socially, had offered to visit him in the hospital. Before I left, a call had been made and Mark had agreed to come in the next morning prior to Karl’s return visit to Peterborough for his late-afternoon operation.
From midnight on, he was allowed no food or water until after the surgery.
Thursday, June 23 – I arrived at the start of visiting hours to find Karl and Mark close to the end of a long conversation and both were relaxed and smiling. They’d discussed everything from the roots of the world’s religions (academically, Karl was well informed) to the mysteries of depression, a whole new and unfamiliar frontier. I could tell the conversation had been helpful and hoped it would give Karl strength to get through a challenging day. He was to travel to PRHC by ambulance, have the surgery, and return to CMH after visiting hours in the evening. Both Karl and the nurses urged me to go home and have a rest as I wouldn’t even be allowed to see him in the recovery room. We were both cheered by the possibility that if all went well, he’d be able to come home the next day.
It was what we both wanted but secretly I wondered how we’d be able to cope.
Friday, June 24 – Excerpt from my update to family and friends:
“After four nights in our local hospital Karl finally had his operation at 7 last evening. There were delays before and after so he didn’t make it back to Campbellford until 3:30 a.m. As nurses come in to wash the guy in the other bed at 6 he had roughly two and a half hours of sleep, pretty much his nightly average for the week.
“He was exhausted and having blood drawn when I arrived at the hospital this morning and is sporting yet another plaster cast, although this one is much lighter. It’ll be replaced by something more streamlined when we go back to see the surgeon two weeks from today. His vitals were all good and after a lot of effort he managed to sit on the edge of the bed and get his legs moving so the doctor said he could go home if the physiotherapist signed off. She’d been concerned about the stiffness and sensitivity in his legs and had asked a neurologist to have a closer look at last Sunday’s MRI but there’s nothing dire showing up on the imaging and both she and the specialist are now suggesting that the mobility issues are all related to the spinal stenosis. The orthopedic surgeon in Kingston will give us a more detailed analysis when we eventually see him. It’s obvious to Karl and me that both the spasms and the stiffness are also exacerbated by stress because as soon as the physio took him for a couple of halting walks and said he could go home the spasms magically eased.
“Our friend Glenn stayed home from his cottage today so he could help me get Karl into the house and I called him at 1:30 to tell him it would probably take about an hour for the discharge.
“That’s when everything started to go pear-shaped. I had spoken to the floor doctor just before she left for the weekend and she’d promised to sign off on the discharge but at 3 p.m. we were still sitting there waiting. The physio had told us we’d be getting a commode, a wheelchair and a four-footed cane on loan and that someone would help Karl down to the car but nothing and nobody arrived. Turns out the doctor hadn’t processed the discharge as somehow the physio’s report hadn’t been sent to her before she left. In growing despair I went down to the Foundation office where our friend John, the executive director, was packing up to depart for the weekend as well. He sprang into action and asked the nursing supervisor to track down the doctor on her cell phone but there was no answer for yet another hour. At long last she replied, approved the discharge papers and ordered a prescription Karl needed so we ended up leaving about 4:45. However, none of the promised equipment turned up and I’d had to call Glenn and let him off the hook as he had an evening commitment.
“Our builder Dave stepped into the breach and met us here for the painstaking process of getting Karl into the house. We had to pretty much lift him onto the seat of the walker so we could push him into the living room and man-handle him into the lift recliner, where he’s now stretched out for a desperately needed sleep. He’s under-fed, dehydrated and completely done in but very happy to be home so I’m hoping that after a night in the comfy chair he’ll be able to manage an assisted walk to the bedroom and bathroom. I picked up a portable urinal on the way home so that will have to do in the meantime.
“We’re both exhausted and it could be argued that he probably should’ve stayed where he was for one more night. But as I said to the doctor, I had to weigh the physical risks against the emotional ones and Karl badly needed to be out of that noisy, confined environment.
“We’ve had a light dinner I’m keeping the liquids flowing to him and we’ll just muddle along. He’s had one shower in six days and could really use another but we’ll worry about that tomorrow. Things are beautiful at the River and that will be a welcome tonic.”
Discharge summary notes: Patient presented with lower back pain, recurrent falls and right wrist fracture after a fall. He reported lower back pain, lower back muscle spasms and falls after the big storm when two trees fell onto his roof and he did a lot of heavy lifting cleaning the debris. On presentation he did not have any neurological deficit. An MRI of lumbar spine was done on June 20 which showed severe facet joint osteoarthritis and multilevel moderate to severe lumbar spinal canal stenosis mostly noted at L4-L5 disc space. A consultation was done with neurosurgery service at KGH; neurosurgeon suggested that lower back pain is mostly secondary to severe facet joint osteoarthritis. No urgent intervention suggested. Dr. suggested follow-up with him as an outpatient for consideration of elective lumbar decompression. Referral was sent. He was treated with topical and systemic analgesics and muscle relaxants during hospital course and was also assessed by physiotherapist.
There is a transverse, comminuted and displaced intra-articular fracture of the distal radius with posterior displacement and angulation. There is a vertical and displaced fracture of the ulnar styloid process. He had ORIF right wrist June 23 with no complications.
Saturday, June 25 – Karl’s night in the chair and mine nearby on the living room couch had been a surreal interlude of mixed emotions – for him, elation at being home combined with deep frustration about his dependency; and for me, hope that his raised spirits would lift the depression, mixed with abject fear that I wouldn’t be able to move him by myself. None of the promised equipment from Home Care had been sent home with us and before I turned out the light, I emailed a nearby friend who’s a physiotherapist to ask for guidance. Doreen and her husband had been away for most of the year on an exciting retirement adventure but she knew of Karl’s challenges and arrived like ray of sunshine in the morning, her car loaded with a footed cane, a strong but lightweight transfer chair and various therapeutic accessories. Between us, we got Karl comfortably settled in the chair and I was able to wheel him into his beloved office, where he finally fired up the desktop after a week away. Constant online contact with many close friends had been a lifeline for him since the beginning and being back at his desk at least gave him the illusion of more control.
A short time later our builder Dave called to ask if he could help with anything and I took advantage of his size and strength to help me get Karl into the shower (cast enclosed in a plastic bag) for his first proper wash in five days. Dave left but came back a few hours later with some little wooden ramps he’d whipped up in his shop so I could maneuver Karl out onto the deck in our beautiful summer weather.
We still had no commode chair and despite our “comfort height” facilities in the house there was no way I could manhandle him onto the toilet, so I just drove into the pharmacy in Campbellford and bought one – cheaper than I’d feared at $83 but worth its weight in gold for peace of mind. Karl could then hoist himself out of the wheelchair with his left hand – blessedly, his dominant one – and stand at the sink while I swapped the wheelchair for the commode. I commented to a friend by email, “So far the meds are keeping him completely bunged up but now that he’s home and off the hospital food something major could happen at any moment!” For Karl, the prospect of me having to clean both him and the commode after a bowel movement was the pinnacle of mortification, second only to a young female PSW seeing him nude in the shower. For me, it was a moment of elation at that one simple achievement. I could never have even pictured it when we were both healthy and mobile.
An even bigger challenge was figuring out the most logical way to help Karl from the wheelchair to the bed and vice versa. He had to lean over and grab the handrail on the bedside, haul himself up with my help and swivel his backside far enough onto the bed that he wouldn’t slide down onto the floor after I pulled away the wheelchair. In reverse it was a much more daunting task, demanding that I get the chair at just the right angle and firmly secure it with my body so it wouldn’t move during his often-erratic lunge from the mattress onto the seat. We were both terrified, which didn’t help, but eventually managed it with a few bruises for him and strained muscles for me but no serious crashes. I was grateful we both had plenty of upper body strength.
In a note to friends later that day I summed up our state of mind: “We’re trying to count our blessings and I’m well and strong (nothing like a messed-up husband to take your mind off a long-Covid headache) but all of this has been sheer hell for Karl and he’s struggling to keep up his spirits. He’s started pointing out dust bunnies for me to vacuum, though, so I’m pretty sure it’s not clinical depression. We have a phone meeting with our wonderful GP Brendan on Tuesday and are hoping for a not-too-distant appointment with a neurologist but in the meantime I think sleep, peace and quiet and the love and concern of all our friends will mean incremental improvements every day.”
Monday, June 27 – My note to Linda after Karl’s two full days at home: “I’ve been impressing on Karl the need to properly rest and we thought today would be the day but we got an early call from a PSW named Amanda who said she’d be here at 10:30. Apparently we’re incredibly lucky to get two PSW visits a week so we rushed to get ready and after a get-acquainted chat she gave Karl a shower.
“She was strong and skilled and it was an opportunity not to be missed! After that, UPS showed up with a forearm walker I’d ordered from Amazon when we learned he’d be in a cast for weeks and against my better judgement Karl was eager to give it a little test. We can tell it will work wonderfully when he’s more recovered from his fall but the effort really tired him.
“We then regrouped to get ready for a phone appointment with Brendan at 2 p.m. and it was excellent too. He was shocked and sympathetic about everything that’s happened in the last couple of weeks and is pulling out all the stops to get Karl into the neurosurgeon as soon as possible. Apparently, this specialist in Kingston is terrific and Brendan promised to call his office directly. Oddly enough, he didn’t seem excessively concerned about the spinal stenosis details in the MRI report and even hinted that the severe mobility problems might not have anything to do with it! He believes it's some neurological anomaly and is keen to get the sort of nerve induction testing that will tell the tale. Best of all, he said ‘Don’t worry, Karl, of course you’ll be fit and well again’. He told me to send him all of the messages I’d emailed to friends and family so he’d have the entire detailed story and asked to be put on the list for updates.
“We confided in him about Karl’s new struggles with the blues and Brendan assured him that almost everyone who has a debilitating back problem gets depressed and ‘catastrophizes’ about the spectre of never walking again. All of this should have, and did, cheer Karl up tremendously but as the day goes on and he gets more tired the dark thoughts descend and he obsesses about a bleak future.
“I reassure him until I’m blue in the face and exhausted myself but today he really sank into the abyss. The upshot is that he gets electrical jolts that are probably what they used to call an attack of nerves but they literally jerk him around and even make him jump and spill things while he’s eating. He was outside on the deck while I was doing a few garden chores and I heard him answer the phone to an arborist we’d called about tidying up some of our trees. Two sentences into the conversation he had a huge spasm that sent the wheelchair shooting back and made him call out to me in a panic. I took the phone and finished the call but it was worrying to see him so shattered and I wasn’t able to truly calm him down until bedtime, when he stood at the sink and flexed his legs before transferring easily into bed and doing a few impressive leg lifts and bends. There’s some kind of head game going on and I only hope it will start to pass as he feels better and before it does my own head in!
“I don’t feel I can leave Karl at the moment so I’m taking a local friend up on her offer to come and sit with him while I go out to grab a few groceries before coming back for what I sincerely hope will be an afternoon of complete rest for Karl and nothing more than garden watering for me. A massage therapist is coming from Campbellford next week to give Karl a treatment after which my hairdresser Teri will arrive and cut his hair. We’re also hoping the physio visit promised by Home Care will happen between now and then.”
It wasn’t until a few days later that Linda, an inveterate researcher of medical conditions, told me she’d been online for days looking at motor neuron conditions and searching for answers. I’d quietly been doing my own scrolling and heaved a sigh of relief every time the common symptoms of one frightening illness or another failed to match Karl’s experience.
Later that day I sat down at my computer to write the following list of “points to remember” that I would subsequently make Karl read several times a day in hopes that it would give him a bit of comfort and perspective:
All your vital signs are consistently excellent
All doctors and physios have been impressed with muscle tone and flexibility in your legs
Two doctors and two physios have told you that spinal stenosis at the level of yours can be controlled and won’t interfere with your lifestyle
Your fears and emotions are legitimate – in the last three months you’ve endured a life-threatening bacterial infection, cancer scare, endless tests, eight days in hospital, storm damage to the house, nine falls at home, a badly broken wrist requiring surgery and the death of one of your closest friends
You have a solid network of family and friends who love you, are cheering for you, are eager to help you and want only the best for you
You have a safe, comfortable home adapted well for temporary disability and caregivers who are available to treat you
Your medical care and attention have been unsurpassed
We have the means to buy anything you want or need to aid and speed your recovery
Your hip pre-op will be rescheduled for August and replacement surgery will follow
Holidays are pending in Europe and the Dominican Republic
NO-ONE HAS GIVEN THE REMOTEST INDICATION YOU WON’T MAKE A FULL RECOVERY!!
I must’ve believed my own messaging too. In retrospect, it’s obvious that despite my worry and moments of hopelessness as I watched my happy, healthy husband shrink and lose his spark before my eyes I had a deep conviction that he’d recover as he always did. At worst, I was afraid that he might not regain his full mobility and would have to rely on a walker, something I knew was his darkest fear as well. Over and over in the final weeks Karl would ask me, “Do you think I’ll ever walk normally again?” I finally said “Yes, of course I do. And if not, you don’t need to worry. I love you more than anything in the world and I’ll always be here”. It was the closest I’d come to admitting to him or myself that the road ahead could be long and painful. But neither of us - even once - had the remotest notion that he could die.
Around this time, I thought back to one of our later appointments with Brendan when we’d been talking about the load Karl was carrying and I remarked “but despite everything, he’s still relentlessly cheerful”. It was one of my typical descriptions of Karl but Brendan seized on it with a cautionary frown, warning that Karl mustn’t feel obliged to be cheerful if bravado was covering up some deep-seated pain and fear. He needed to remember he wasn’t a soldier anymore. We’d left the office with a prescription for Valium, hoping for any small change that would ease his tortured mind.
Apart from lying in bed and standing at the sink, Karl was spending all of his time in the wheelchair, including for meals and evenings in front of the TV. His one night in the lift chair had been his last. And as each day wore on he’d spend time seeking comfort from concerned friends via email and phone with bouts of crying in between. It helped him to have a conversation about depression with another Ashford Hollow neighbour, a retired U.S. Marine who’s fought a long battle with PTSD, but Karl’s nights were fraught and full of flashbacks to dark memories. He started to call out in discomfort and agitation several times during the night and I would get up repeatedly to help him shift position and hold him until he could fall into another troubled sleep. He hated to disturb me and I was worn to a frazzle by frustration and exhaustion. Yet I still insisted on hoping for the best.
A big part of the problem was the involuntary spasms that would hit Karl out of the blue and make it impossible for him to fully relax or have a proper meal. I’d taken to holding his wrist while he tried to maneuver a bite of food into his mouth but the muscular intensity of the spasms often defeated me as well. He came close to stabbing himself in the face with a fork and would often bite down painfully on a spoon. We longed for the day when the right drug or proper course of treatment would finally kick in.
One of our closest friends, who spends weekends with his partner at their Prince Edward County cottage, is a Toronto-based psychiatrist. When Karl said he wanted to have a long talk with Martin, I asked if they could find time for a visit.
Thursday, June 30 – We still hadn’t heard from Home Care about an OHIP-assigned physiotherapist for Karl so our physio friend Doreen offered to take a break from retirement and give him some treatments. While Karl’s difficulties getting in and out of the chair were still plaguing us, we were at least more rested and relaxed at home and when Doreen arrived late morning Karl was up, washed, shaved and in his t-shirt and gym shorts. After an initial analysis of his ability to stand at the kitchen counter and move along it without assistance (slow and painstaking) Doreen suggested we go out to the deck and run through a series of about 15 exercises for Karl to perform in daily routines.
She continued to be impressed with the muscle tone in his legs as he handily managed squats, extensions and sideways steps while gripping the deck railing. He was too nervous to ease his grasp, though, and even balked at putting the arm in the cast on one of our shoulders while using just one hand on the rail. He seemed energized as he worked through the motions, though, and Doreen smiled and encouraged him while declaring he’d be going up and down the three steps to the deck within two weeks. We both felt a rare small wave of hope wash over us.
We made another appointment with her for the following week and over the next few days Karl was feverish about going through all 15 exercises, half outside and half on the bed, twice daily. I coached him through the lying-down leg raises, circles and bicycle motions and we did the outdoor squats, lunges and stretches together. He felt discomfort but no pain and I marveled at his strength and flexibility while lying on his back or holding on to the deck railing. His broken wrist was clearly on the mend and the strength in his fingers was returning. Afterwards I’d bring out a basin of soapy water and a face cloth, help him strip down at the railing and in glorious sunshine I’d give him a thorough wash followed by a rinse with the hose. Afterwards he’d sit at the outdoor table for a shave and a long session with his iPad. It wasn’t until later we found out he was meant to work his way through the exercises gradually over weeks, not all at once, but the workouts were a rare boost for both of us and it felt like a ray of sun coming out after the storm.
At that point neither of us knew that we’d never find out if Doreen’s two-week promise would be fulfilled.
Friday, July 1 – Sunday, July 3 - Our usual Canada Day routine was to have Linda, Arthur, and their dog to our house on the river along with several other friends from near and far for a celebratory day of food and fun while we watched the cruisers go by. This time the weather was perfect but we couldn’t manage any visitors that weekend except Murray and Martin, who arrived as planned for lunch on the Sunday.
Like many others who hadn’t seen Karl for several weeks they were deeply shocked by his weight loss and the wheelchair. He’d never sat for the arrival of guests in his life and although he joked about it and tried to be entertaining we all knew his smile was masking despair. In the previous few weeks his animated face had also undergone a change with a faint droop to the corner of one eye and lips that were slightly off centre. We enjoyed a largely spasm-free lunch, though, and Murray and I sat on the lawn for a chat while Karl bared his soul to Martin. Afterwards I wrote the following recap to a friend in the U.S.:
“We haven’t been having visitors except for physios and PSWs but today our dear friends Murray and Martin brought lunch and we had a lovely catch-up on the deck. Martin’s a psychiatrist and we wanted his take on Karl’s recent bouts of the blues and frequent, previously unheard-of crying jags - understandable given all he’s been going through. He’s typically so active that spending most of his time in a wheelchair is deeply upsetting.
“Martin concluded he is suffering from PTSD and clinical depression and suggested that now that Karl’s course of Valium is over we ask Brendan for an anti-depressant instead.”
Monday, July 4 – Brendan complied with Martin’s recommendation but as usual, Karl was a poor candidate for any strong drug and the first one flattened him, causing disorientation, blurred vision and dry mouth as well as a continuance of some mild hallucinations that we’d blamed on the Valium and the cornucopia of drugs he’d had in the hospital. He persevered for three nights of emotion and nightmares before giving up and reverting to Tylenol PM. That night I joined him in the guest room bed in hopes that it would help calm him and it was a comfort to both of us.
Tuesday, July 5 – Karl felt better after a PSW came to give him a shower in the morning and at long last Rohan, a very nice physiotherapist from Peterborough, arrived for an appointment booked by Home Care. He examined, tested and analyzed Karl in much the same way Doreen had and came to a similar conclusion. Apart from the obvious balance problems and diminished muscle mass from his sudden weight loss, there was no apparent obstacle to Karl regaining his mobility over time. He was concerned about the precarious process of transferring him in and out of the chair and bed and gave us a couple of helpful tips but had no further ideas. Rohan recommended another course of exercises for Karl to undertake gradually and with caution and promised to return the following week.
As usual, an optimistic prognosis was a boost for both of us but everyone’s inability to pinpoint exactly what was going on with Karl continued to erode our confidence and dampen our hope.
Around that time our friend John, who’d been so helpful the day of Karl’s hospital discharge, called him to ask if there was any way the two of us could attend the annual Doctor’s Cookoff, a hospital fundraiser scheduled for Friday the 8th. We’d made a large donation as a thank-you for the great care at CMH and John, who was executive director of the hospital Foundation, wanted us to kick off the proceedings. Karl said it would be embarrassing and next to impossible for us to manage the wheelchair at the open-air event but insisted that I would go. He said, “Janice desperately needs a break” and promised that he would be fine at home in the chair with the TV, his iPad and the phone. I agree to attend for no more than 90 minutes and Karl made plans for Friday evening phone and Face Time calls with some close friends.
Wednesday, July 6 – It turned out to be a full day, as Doreen at arrived at 9 a.m. for another physio session followed by an in-house massage courtesy of a lovely therapist from Burnbrae Health. She set up her table in the kitchen and helped Karl out of the chair and onto it with strength and confidence. I could tell that such targeted, cheerful attention from caring women was a tonic for him and by the time my hairdresser Teri arrived at 2 p.m. to give Karl a much-needed haircut he was smiling and visibly more cheerful.
It had been a good day and we were both looking forward to his Friday appointment with the orthopedic surgeon at PRHC, at which the awkward plaster cast would finally be replaced with a lighter, more comfortable brace. Karl had no pain in his wrist and over the previous couple of weeks had been using his right hand more normally and feeling the strength come back. Since Doreen was optimistic about the progress of the physiotherapy, I’d called the hip surgeon’s office to confirm a date for the replacement at the end of September. When he was given a late August pre-op appointment, Karl finally had something to look forward to.
Thursday, July 7 – In anticipation of our car ride to and from Peterborough the following day, I’d talked to the PSW who was due to come that week and she’d agreed to arrive early on Friday to help Karl with a shower, then assist me in getting him out the door, down three steps and into the passenger seat. We had a plan and settled in for a pleasant day in the sunshine. Later an email arrived from our American friend Betty, Terry’s widow, to let us know she was thinking of us and I sent her the following reply:
“Lovely of you to check in and I really appreciate your thoughtfulness. Things are difficult as Karl’s become a full-time job and there aren’t many opportunities for a break but at least the weather is lovely and we’re able to spend time on the deck. We’re lucky to have physiotherapists on board and Karl has made quite a lot of progress but the clunky cast is still throwing him off balance. Hoping he gets something lighter and easier when we go to Peterborough for a follow-up with the surgeon tomorrow.
“We’re thinking of you too and Karl’s goal is to be walking to Terry’s celebration of life next month, even if it’s with a walker or a cane!”
Friday, July 8 – Excerpt from my email update to family and friends at 4:30 p.m.:
“Today started with a wave of panic as the PSW who’d promised to arrive early, give Karl a shower and help him into the car for our mid-morning hospital appointment failed to show up and didn’t answer her cell phone! We finally made do with a sponge bath and my nephew Rob, who just happened to be at his mother’s cottage up the river, came to the rescue within five minutes. His twin brother Jeff then raced to his own cottage to repeat the favour when we got home.
“We had already had a call from the hospital first thing this morning to let us know that their online systems were down because of a massive Rogers Communications outage and it could be a chaotic visit but as luck would have it, the tech failure had the opposite effect. Countless appointments were cancelled and waiting rooms were mostly empty so Karl had his post-surgery cast removed, got an
X-ray and had the consultation with his surgeon within 90 minutes.
“We were enjoying a rare moment of elation until Dr. Wong looked at the X-ray and noticed that a small bone had moved out of place in the last two weeks – not Karl’s fault, he was quick to assure us. Unfortunately, the upshot is that Karl has to go back to PRHC on Sunday for another operation, although this one will be fairly minor and he’ll be able to leave with the lighter and easier Velcroed brace they put on him today.
“It sucked all the wind out of our sails instantly but at least the doctor said he couldn’t see any reason why Karl shouldn’t have his hip surgery six to eight weeks down the road. We’re not likely to get a date that quickly but it’s a relief to know he can finally go back on the list! Karl’s referral to a neurosurgeon in Kingston for an assessment of any other possible damage to his spine is also in the works as we got word that his appointment will be scheduled in one to two months.
“Obviously it’s not the summer we pictured and our spirits are bouncing up and down like worn-out tennis balls but our health care providers continue to be amazing and the support and concern of all of you is the best tonic on the market!
“My fervent wish is that my next update will be the last, and only one short paragraph with news that he’s the picture of health and rarin’ to go.”
Shortly after we returned from Peterborough and my nephew Jeff had teased some laughter out of Karl as we maneuvered him into the house, we had an unexpected phone call from our other PSW Amanda, who’d heard about her colleague’s failure to show up and insisted on coming over to give Karl his overdue shower.
We were both pleased to see her but Karl was exhausted as they made their way to the bathroom. They’d shooed me away to make some tea but before I could reach for the kettle I heard a crash from down the hall and both of them calling my name. While Amanda was trying to help Karl back out over the lip of the shower enclosure, he’d lost his balance and both of them ended up on the floor. Karl was unhurt and trying to see the funny side of the situation but I could see panic mounting as he worried that the two of us wouldn’t be able to lift him up. That might’ve been true just three months before but we each took an arm and handily lifted him into the wheelchair. Amanda and I were both shocked at how it was done in one easy, fluid movement. He felt as light as a feather. I calculated his weight loss to be at least 20 pounds.
After Amanda left, we went out on the deck so Karl could shave and catch up on email and passed a couple of pleasant hours in the sunshine before I had to leave for the Doctor’s Cook-off. The stress of the day was catching up with Karl, though, and when I settled him in the living room and took him a small bowl of pasta for dinner he could barely get through half of it. As I dressed for my first social outing in weeks, I nearly changed my mind about going but Karl insisted. He had a portable urinal and the TV remote within reach and said he’d be calling friends in Uxbridge and Michigan while I was gone. As usual his mental faculties were sharp and consistent, yet another reason I never feared the worst.
I returned about 8 p.m. with a delicious plate of strawberry shortcake the auxiliary had sent home for Karl and he managed to eat most of it while I told him everything that had gone on at the event.
He pretended to be interested but it was obvious he wasn’t focused and at 9 p.m. he said he wanted to go to bed. Surprised that he chose to go so early and promising to join him within an hour, I asked if he was feeling ill. He said “No, I just feel detached”. It was a curious remark that came back to haunt me in the hours ahead.
Saturday, July 9 – When I’d finally climbed into bed with Karl, I found him awake and in discomfort as he tried to find a workable sleeping position. We both tossed and turned until about 2 a.m. when I finally helped him roll onto his side and curled in behind him like a spoon, resting my hand on his leg. He seemed elated and said “Thank you Darling, that’s so much better. I feel good now.” We both fell asleep within moments.
I was disoriented when I woke up with a start at 5 a.m. and wondered if something had fallen onto the floor. Instead, I realized it had been a violent motion on Karl’s part and raised myself on an elbow to check on him. He was on his back, completely rigid and immobile, with his eyes open and the same panicked expression he’d had when he couldn’t breathe weeks earlier. I asked what was wrong and through clenched teeth he uttered “Nightmare”. Once again, I urged him to take steady breaths through his nose but while he tried, it was no use. My fears mounted as I desperately tried to remember the basics of CPR and realized in desperation that there was no phone in the room.
I straddled him and started chest compressions and when he closed his eyes and seemed to pass out I pinched his nose and clumsily tried to blow air in through his mouth. Finally realizing I had no other option I raced into our bedroom and back for the phone and called 911. The dispatcher told me to resume compressions but at that point I was in tears and overwhelmed with the fear that it was too late. I also realized the deadbolt was on the door and the paramedics wouldn’t be able to get in. The dispatcher, a calm and kind woman, told me she’d let me know when the ambulance was at my door and that I should continue pumping his chest until they arrived. If Karl was still alive at that point the final words he heard me say were: “Don’t you dare leave me”.
The next hour was a blur after I was given the signal to run and unlock the door. The fire team arrived first with the paramedics on their heels and as men and women raced to the guest room, hauled Karl up by the bed sheets and laid him out on the dining room floor I sank onto the bed in our room and listened to machines and medics try for what was probably half an hour, but seemed like twice that, to save his life. I later discovered in the post mortem that all his ribs had been broken in the attempt. Everyone did their utmost but deep down I sensed that Karl had been gone before they’d arrived.
When a young firefighter came in to ask if there was anyone I wanted to call, he confirmed out loud what I already knew but was desperate to deny. At 5:50 he dialed my nephew’s cell number and handed me the phone. I heard myself breaking the news to Jeff, who arrived minutes later to drive me to the hospital in the wake of the ambulance crew that carried Karl out of our home for the last time.
The aftermath, and a deeper mystery
Later that summer, after a whirlwind of emotional calls and visits from friends, gut-wrenching meetings with funeral directors, lawyers and investment advisors and more bouts of tears than I ever thought possible, I sat down to pour out my heart in a journal entry:
“It’s Saturday morning August 14th, exactly five weeks since Karl woke from a nightmare unable to breathe and died in my arms. Five weeks that are like five minutes, five months, five years and five lifetimes all at once.
“Widow, that word that applies to old women, women in war-torn countries, women in care facilities, women drained and weary from caring for partners with long illnesses is now the box I’ll have to check on official documents. It’s a word I believed would never define me as I was pretty sure my lively, energetic, med-free, heart of an athlete, relentlessly healthy husband would outlive me. He was 71 when he left me without warning five weeks ago and I’m 69. Not spring chickens by any means but secure in our determination to have at least another decade of travel, entertaining, house projects, fun with friends and our usual cozy companionship before we ever had to think about getting old. Ten years of my life I would gladly give away if I could just have him back for one day.
“Both my strength and my weakness have taken me by surprise since it happened. The first minute, when I realized all my frantic efforts to save him were futile even before the army of paramedics, police and firefighters raced in to intubate, pound and shock him back to the life that was already gone; en route at dawn to the hospital with my nephew Jeff to find the emergency room doctor standing in the doorway to meet us with profound sadness in his eyes; going into the treatment room where Karl lay peaceful and motionless on a gurney and noticing how great his hair looked after Teri’s home visit; sitting in a hospital family room with a sympathetic policewoman and my minister, who’d appeared out of thin air; giving my nephew instructions about who he needed to call right away; agreeing with Dr. Elia, and upon Jeff’s urging, to request a post mortem in light of a death with no discernible cause; and returning home on a beautiful July morning with dear friends, caring neighbours and tearful family gathered on our pretty lawn on the river to weep, hold me and quietly speculate on how this could possibly have happened. It felt like strength at the time and I was grateful and inexplicably calm.
“Shock, of course, or was it? I reflected on how often suddenly bereaved people say, “It hasn’t sunk in yet” and realized I wasn’t one of those. Karl had died in our bed while I was pinching his nose, trying to blow breath into him and applying endless chest compressions to no avail and the end of his life is seared into me like a brand. Five weeks later I still haven’t had the wrenching experience so many do of waking from sleep thinking everything’s normal, only to relive the nightmare of his passing. I have no delusions or illusions. He’s gone and I’ll never see, hear or hold him again. This page is now blurred with tears and the choking sobs have begun.”
Karl and I had both elected cremation in our wills but before his could be arranged his body was transferred to Kingston for the post mortem, which was performed a few days after his death. I was told the report would be sent to Dr. Elia at CMH within a month but it ended up taking five and I didn’t get an explanatory call from the doctor until December. The news wasn’t worth waiting for, though, as the post mortem revealed no clear answers to why Karl contracted all of his bizarre symptoms and no explanation for how or why he died. The word “unremarkable” appeared 32 times in the report. Even the natural assumption that it was a pulmonary embolism that finally killed him was shot down as there was no evidence of a blood clot in his system.
Our own GP later theorized that it was probably a heart spasm that actually ended his life. I’d never heard of such a thing but apparently it often happens to people with severe stress but no history of heart disease and after one violent and deadly contraction, leaves no telltale evidence to confirm its presence. When I thought of Karl’s terrified expression at the end and remembered my fleeting notion that he was dying of fright, this seemed like the most logical explanation.
The cremation had taken place mid July and as I was planning a celebration of life but no funeral service the undertaker placed the velvet bag with Karl’s ashes in my “urn” of choice, a handsome redwood humidor lined with cedar and sporting a brass plaque with “Karl Eichner” on the lid – a going-away gift from his staff when he left Canada News-Wire. It remains on a living room shelf today.
It was in mid August, around the time I wrote my journal entry, that I was sitting in my home office dealing with all of the paperwork that lingers for months after a death. The phone rang and call display indicated a local number so I picked it up, expecting it to be a call from a friend.
Instead, a man’s voice I didn’t recognize said “Is this Mrs. Eichner?” When I affirmed it, he said “My name’s Ron and I live in Campbellford. Actually, it’s your husband I wanted to speak to if he’s available.” There was silence at the other end of the line when I told him why that wasn’t possible and after a few moments he went on to explain. Apparently, he’d read the article I’d written for the hospital foundation newsletter back when Karl was making a slow but seemingly full recovery from the bacterial infection and he was now calling to compare notes. He said, “I wanted to talk to your husband because of what happened to me a few months earlier.” I listened in shock as he related the story of how he’d wakened with exactly the same violent leg spasms that had rendered Karl immobile in April. He said he lived alone, though, so immediately called an ambulance and was subsequently admitted to CMH when there was no immediate explanation for the symptoms. He stayed for a month while gradual deterioration of his mobility took him from a cane to a walker to a wheelchair. The baffled doctors ran test after test and finally referred him to a neurosurgeon in Kingston.
Like Karl, he had both brain and spinal MRIs and while the surgeon in Kingston identified a small benign tumor in Ron’s upper spine and removed it surgically, he admitted there was no clear evidence of any relationship of the tumor to the crippling spasms. Ron spent several weeks afterwards in a rehabilitation facility before he was eventually sent home with no clear answers. When I asked how he was, he said, “I’m a little better but still using a walker.”
If I was stunned by the story to that point, I was absolutely gobsmacked by what came next. I told him about Karl’s customary good health and while Ron admitted he wasn’t as healthy in general as Karl had been he said that prior to the spasms he was still walking around the canal in town every day. He then mused about the “only other weird thing” that had happened to him in recent years – a few weeks in which he lost consciousness five or six times for no reason. I listened in disbelief while he described an experience that mirrored Karl’s in the summer of 2018 – the initial assumption that he was having an electrical problem in his heart, the temporary loss of his driver’s licence while he underwent a long series of cardiac and neurological tests that revealed nothing and the ultimate conclusion in the absence of any other explanation that the episodes were caused by “stress”. As the conversation came to an end, I thanked him for his call, wished him well and asked how old he was. “I’m 71”. We haven’t spoken since but when I recently called his number to ask if I might use his last name in this story, a recording told me it was out of service. Needless to say, I fear the worst.
The subsequent two and a half years have melted away and my life often feels like a documentary I’m watching on a screen. There have been three wonderful celebrations of Karl’s life -- locally, in Ellicottville, NY and in Karl’s home town of Bangor, Northern Ireland -- and gifts in his will have benefited CMH, the Peterborough Regional Health Centre, the Canadian Canoe Museum, the Ontario SPCA and several other pet causes. Memorial benches in Campbellford and on Ballyholme Beach in Northern Ireland have been dedicated in his memory among many other commemorations. When I learned that “memorializing” has been added to the stages of grief I understood why I was so motivated to keep Karl’s memory alive. Those closest to me have been quick to deny that forgetting him is even a possibility. I’m enormously grateful for their love and concern, as well as for my riverside home that gives me huge comfort and pleasure even if joy is still out of reach.
The need to tell Karl’s story has run deep, though, and if physicians and others are willing to read it, I’m clinging to hope that someone, somewhere, may be able to connect some elusive dots and finally give me a solution to the ongoing mystery of his illness and death. If not, I’ll pray for peace and acceptance instead of an answer at all costs.
If you’ve persevered to the end of this, you have my most heartfelt thanks.
Janice Eichner








I read your entire story with tears in my eyes. I recently lost my husband and although our story was quite unlike yours, there were some similarities. We are older than you and my husband had cancer. But he had always been a very active, hard working man. The trips to hospital, the sponge baths, care workers in the home, sleepless nights and constant worry are all similar. It is definitely a different life without our spouse. They are loved and missed every single day. Thank you for sharing this.
This is a very hard read. I kept going back to it. Is there health care in our community that we are lacking?